In addressing the issue of colon cancer and baby boomers, let’s understand who we are talking about. The Baby Boomer Generation is generally defined as those people born between the years 1946 and 1964. I am in the earliest part of that time frame so this information is of particular interest to me.
10,000 baby boomers reach the age of 65 each day, and the incidence of cancer is increasing among that age group. This is largely due to cancer being diagnosed at a higher rate among us. We are living much longer than previous generations, and the chance of having a cancer diagnosis has also increased. With colon cancer being the 4th most common cancer, it is important to have a good understanding of the risk factors, screening, prevention, and treatment options.
Medical science has brought many improvements in the treatment of most cancers. However, prevention is ALWAYS the best cure!! If you need to make changes in your lifestyle, nutrition, and activity, every day you delay is one more day of increased risk.
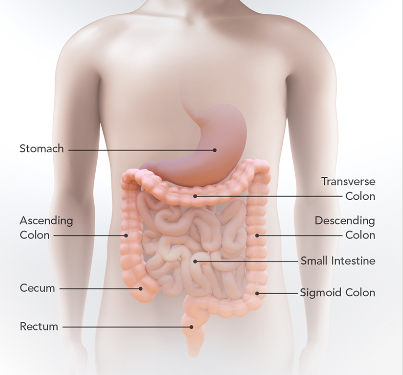
Colon Cancer (often referred to as colorectal cancer) is a disease where cells in the colon or rectum grow out of control. The colon is the large intestine or large bowel. The rectum is the passageway that connects the colon to the anus.
Sometimes abnormal growths, called polyps, form in the colon or rectum. Over time, some polyps may turn into cancer.
Not counting skin cancer, colorectal cancer is the fourth most common cancer in men and women. It is the fourth leading cause of cancer-related deaths in the United States.
Risk Factors for Colon Cancer
The risk of getting colon cancer increases as you get older. Certain risk factors lead to a higher risk. These include:
- A History of:
- A personal or family history of colorectal cancer or colorectal polyps
- Inflammatory Bowel Diseases such as ulcerative colitis or Crohn’s disease
- A genetic syndrome such as familial adenomatous polyposis (FAP) external icon or hereditary non-polyposis colorectal cancer (Lynch syndrome).
2. Lifestyle factors that may contribute to an increased risk of colorectal cancer, including:
- Lack of regular exercise and physical activity
- A diet low in vegetables and fruit
- A high-fat/low-fiber diet, and/or a diet high in processed meats.
- Overweight and obesity
- Alcohol consumption in excess
- Tobacco use (1)
Prevention Of Colon Cancer
While there is no absolute way to prevent colorectal cancer, there are things that can lower the risk. The following recommendations are referenced by the American Cancer Society.
Colorectal Cancer Screening:
First and foremost: Colorectal Cancer Screening to look for cancer or pre-cancer is one of the most valuable tools for both preventing colorectal surgery or identifying it in the early and treatable period.
Because when the first abnormal cells start to grow into polyps, it usually takes about 10 to 15 years for them to develop into colorectal cancer. Regular screening can find these polyps before they have a chance to turn into cancer.
The recommendation is if you’re age 45 or older, you should start getting screened for colorectal cancer.
If there is a strong family history of colorectal polyps or cancer, talk with your doctor about your risk. The physician might recommend genetic counseling to review your family medical history and make further actions.
Weight Management and Exercise
Managing your weight and having regular exercise may lower your risk of colorectal cancer.
Weight: There is no question that being overweight or obese increases the risk of colorectal cancer. and the link seems to be stronger in men. So, maintaining a healthy weight may help lower your risk.
Exercise: Yes, being more active lowers your risk of colorectal cancer and polyps. In addition to regular moderate to moderate to vigorous exercise lowering risk, limiting the amount of time you are sitting or lying down may also be a benefit. Increasing the amount and intensity of your physical activity may help reduce your risk.
Smoking
Long-term smoking is linked to a higher risk of colorectal cancer, as well as many other cancers and health problems. Quitting smoking may help lower your risk of colorectal cancer and many other types of cancer, too. Needless to say, smoking is a habit that contributes to so many health issues. It is critical to your health to stop, or not start!!
Nutrition:
Can your diet impact your health including diseases? Yes! For baby boomers (and other age groups), the risk of colon cancer can be greatly reduced. The old saying, you are what you eat, is true. Processed, fatty, too much sugar and too many carbohydrates can only lead to poor health, low energy, and digestive problems. Not only can this way of eating increase your risk of colon cancer, but it can also contribute to the cause of many other diseases (i.e. diabetes, kidney disease, and heart disease).
A lifetime of poor eating can be reversed, but it needs to happen now before it’s too late and your body already has advanced disease. Make the change in your eating habits before you develop colon cancer, and worse, inoperable colon cancer. So, fight it! Baby boomers: colon rectal cancer can be avoided.
Plant-based foods such as tomatoes, citrus, berries, peppers, carrots, cabbage, broccoli, and soybeans are all foods high in flavonoids, polyphenols, and terpenes which are also beneficial for the avoidance and fight against colon cancer.
Calcium and Vitamin D have been shown to help fight off colon cancer. However, it is thought that nutrition through food is better for your than supplements. Foods such as milk, yogurt, cheese, salmon, sardines, mustard greens, kale, and collard green are great sources of calcium. Salmon, sardines, milk, egg yolks, and chicken livers are also excellent sources of Vitamin D. Another great source of Vitamin D is, of course, the sun; before 10 AM and after 3 PM for the healthiest exposure and only for about 20 minutes each time, is all you need to absorb Vitamin D. However as we get older, our bodies do not convert sunlight into Vitamin D as easily.
You can learn to eat a healthy, cancer-fighting diet by following these guidelines from the American Cancer Society:
- Choose many of the foods you eat from plant sources.
- Eat whole grains rather than refined ones whenever you can.
- Limit your red and processed meats.
- Be physically active; achieve and maintain a healthy weight
- Limit consumption of alcoholic beverages.
Vitamins, Calcium, and Magnesium
Some studies suggest that taking a daily multivitamin containing folic acid, or folate, may lower colorectal cancer risk, but not all studies have found this. In fact, some studies have hinted that folic acid might help existing tumors grow. More research is needed in this area.
Some studies have noted that vitamin D, from the sun or foods (as discussed above), or in a vitamin pill, might lower colorectal cancer risk. Studies have shown that low vitamin D levels are associated with an increased risk of colorectal cancer in addition to other cancers. However, more studies are needed to determine if increasing vitamin D intake from a supplement can help prevent colorectal cancer. Avoiding a low vitamin D level may be helpful; as with other suggestions here, getting advice from your physician is important.
Low levels of dietary calcium have been linked with an increased risk of colorectal cancer in some studies. Some studies note that increasing calcium intake may lower colorectal cancer risk. Calcium is important for a number of health reasons aside from possible effects on cancer risk. But because of the possible increased risk of prostate cancer in men with high calcium/dairy product intake, and the possible lower risk of other cancers like colorectal cancer and breast cancer.
Calcium and vitamin D might work together to reduce colorectal cancer risk, as vitamin D aids in the body’s absorption of calcium. Still, not all studies have found that supplements of these nutrients reduce risk.
A few studies have found a possible link between a diet that’s high in magnesium and reduced colorectal cancer risk, especially among women. More research is needed to determine if this link exists.
Non-steroidal anti-inflammatory drugs (NSAIDs)
I find it interesting that many studies note that people who regularly take aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Motrin, Advil) and naproxen (Aleve), have a lower risk of colorectal cancer and polyps.
But aspirin and other NSAIDs can cause serious or even life-threatening side effects, such as bleeding from stomach irritation or stomach ulcers, which may outweigh the benefits of these medicines for the general public. For this reason, the American Cancer Society does not recommend taking NSAIDs just to lower colorectal cancer risk if you are someone at average risk.
Still, for some people in their 50s who have a high risk of heart disease, where low-dose aspirin is found to be beneficial, the aspirin may also have the added benefit of reducing the risk of colorectal cancer.
Because aspirin or other NSAIDs can have serious side effects, check with your doctor before starting any of them on a regular basis.
Screening For Colon Cancer
Colon cancer screening saves lives. Screening can find precancerous polyps. These are abnormal growths in the colon or rectum. They can be removed before they turn into cancer. Screening also helps find colorectal cancer at an early stage, when treatment works best. About nine out of every 10 people whose colorectal cancers are detected early and treated appropriately are still alive five years later. (1)
Turning 50 is often considered a significant milestone in one’s life. As we age, we become more familiar with the ever-growing list of health issues affecting us. One specific health concern is colon cancer. Effective screening is the best way to detect colon cancer early. While regular mammograms and skin cancer checks are fairly easy to do on a regular basis, colon cancer screening is something that many avoid doing or even talking about.
Colorectal cancer is often considered the most preventable, yet least prevented cancer. The message here is: get screened for colon cancer. While American Cancer Society screening guidelines call for men and women at average risk for the disease to begin colorectal screening at age 50, 23 million Americans in that age group are not getting screened as recommended. Thus, increasing their risk of being diagnosed with colon cancer at a late stage when it is much harder to treat.
Advanced colon cancer is preventable because of its slow development in the body over time. Before cancer develops, a polyp—or non-cancerous growth—usually appears on the inner lining of the colon or rectum. The identification and removal of these polyps, through routine screenings, can effectively prevent colorectal cancer from ever forming. Because most polyps and early-stage cancers cause no symptoms, adherence to routine screenings is critical to cancer detection.
Colorectal cancer can be successfully treated when caught early. For those whose cancer is detected at an early stage, the five-year survival rate can be greater than 90 percent. Unfortunately, lack of adequate screening has meant that in more than 60 percent of all cases, colorectal cancer is not detected until its late stages, making treatment difficult and survival rates low. The sad reality is that the five-year survival rate for colon cancer found at a late stage is a mere 12 percent.
Why Do People Avoid Getting Screened for Colon Cancer?
There are a number of reasons why people don’t screen for colon cancer—discomfort, embarrassment, or even fear. Colonoscopy is the gold standard procedure to detect and remove cancerous and precancerous lesions. However, despite its critical importance, some are unwilling to have a colonoscopy because the procedure is invasive and requires bowel preparation. This includes a clear liquid diet and laxatives. Colonoscopy also requires time off from work. Patients are sedated during the procedure, they must have someone available to drive them home from the procedure.
Less invasive tests, such as fecal occult blood tests (FOBT) and fecal immunochemical tests (FIT), are available for patients looking for an alternative screening option. These tests are non-invasive and designed to detect blood in the stool not seen by the naked eye. However, because there are unrelated conditions that can cause blood in the stool. Not all polyps or lesions actively bleed on a regular basis—or bleed at all— these tests may not be reliable on their own for the detection of cancer or precancer.
Another option approved by the FDA is called Cologuard®. Cologuard®gives those who are unwilling or unable to undergo colonoscopy an accurate, noninvasive screening test they can take in the privacy of their own home.
What makes Cologuard® different from other noninvasive colorectal cancer screening tests is that it analyzes and detects both altered DNA and blood biomarkers in the stool that may indicate cancer and precancers. Every day, cells are shed from the colon wall during the digestion process. As part of this process, normal cells, along with abnormal cells from precancers or cancers, are shed into stool as it passes through the colon – it is these abnormal cells that Cologuard® is designed to find. (2)
My provider orders Cologuard® and each year my husband and I receive one in the mail. Within two weeks we see our results posted on our computer. We still get a colonoscopy every 5 years as recommended by our physician.
Colorectal cancer is preventable and treatable if caught early and boomers today are fortunate to have a number of screening options available to them. The message again: Screen for Colon Cancer. At the end of the day, it doesn’t matter which option you choose—after all, the best test is one that is done—so don’t put it off any longer, now is the time to call your physician and receive you screening. (3)
Symptoms
Colon and rectal cancers do not usually produce symptoms in the early stages of the disease. As the tumor grows, symptoms will depend on the location of the primary tumor within the intestine. Individuals with colon cancer or rectal cancer may experience one or multiple symptoms. These may include the following:
1. Blood in the Stool
You may notice obvious blood in the stool, or darker-colored bowel movements, which may indicate that there is bleeding within the intestinal tract or rectum. Sometimes bleeding may be present but not visible. This is called occult (hidden) blood and may not be discovered until a blood test indicates a low red blood cell count.
2. Rectal Bleeding
Bright red blood in the stool typically indicates that there is bleeding in the rectum or colon, which may be a sign of colon or rectal cancer. Hemorrhoids may also cause rectal bleeding. Typically, patients with hemorrhoids experience symptoms that come and go with flare-ups, whereas rectal bleeding caused by cancer usually continues or worsens and is more likely to be accompanied by pain and a low red blood cell count.
3. Changes in Bowel Habits
Changes in bowel habits that can indicate colon or rectal cancer include the following:
- New-onset constipation or diarrhea
- Changes in frequency or size and caliber of bowel movements
- A bowel that doesn’t seem to empty completely
- A stool that is narrower than normal (even as thin as a pencil)
Occasional bowel changes can be caused by a dietary change, disagreeable food, or a viral/bacterial infection. However, if you are experiencing something new and unexplained—and it lasts more than a couple of days—see your doctor.
4. Abdominal Pain and Bloating
Stomach bloating, distention, cramps, or pain in the abdominal or bowel region can be symptoms of colon or rectal cancer. Other conditions may cause these symptoms as well, such as diet-related gastrointestinal distress, Crohn’s disease, or ulcerative colitis. See your doctor if you experience frequent abdominal pain and bloating that does not have an obvious cause.
5. Nausea and Vomiting
Nausea and vomiting can occur if a colon or rectal tumor is obstructing the bowel and inhibiting the passage of liquid or solid waste or gas. Bowel blockage can also be accompanied by painful abdominal cramps, bloating, and constipation.
Nausea and vomiting are symptoms of a range of conditions, which may be benign or serious. If you experience persistent nausea, signs of dehydration, or vomiting that lasts for more than 24 hours, seek immediate medical treatment.
6. Anemia
Anemia is a blood disorder characterized by a deficiency of red blood cells or hemoglobin. In patients with colon or rectal cancer, intestinal bleeding may cause anemia. Depending on the location of the bleeding within the colon, anemia can be the first sign that blood loss is occurring.
Common symptoms of anemia include skin pallor (paleness), increased heart rate, fatigue, dizziness, and irregular menstruation.
7. Unexplained Weight Loss, Loss of Appetite, and Feeling Weak
Losing weight, losing your appetite, or feeling weak are all possible signs of colon or rectal cancer along with many other unrelated conditions. In patients with colon or rectal cancer, these symptoms are usually related. Persistent diarrhea can cause weight loss. Stomach pain and nausea can reduce your appetite so that you don’t consume enough food to maintain your weight. All these issues, as well as anemia, can lead to weakness.
8. Pelvic Pain
Pain in the pelvic area is not common in patients with colon or rectal cancer. If it occurs, it may indicate that cancer has spread to the pelvic area. (4)
Treatment
Treatment for colon cancer is based largely on the stage (extent) of cancer, but other factors can also be important.
People with colon cancers that have not spread to distant sites usually have surgery as the main or first treatment. Chemotherapy may also be used after surgery (called adjuvant treatment). Most adjuvant treatment is given for about 6 months.
The following information was obtained from the American Cancer Society. (5)
1. Treating stage 0 colon cancer
Since stage 0 colon cancers have not grown beyond the inner lining of the colon, surgery to take out the cancer is often the only treatment needed. In most cases, this can be done by removing the polyp or taking out the area with cancer through a colonoscope (local excision). Removing part of the colon (partial colectomy) may be needed if the cancer is too big to be removed by local excision.
2. Treating stage I colon cancer
Stage I colon cancers have grown deeper into the layers of the colon wall, but they have not spread outside the colon wall itself or into the nearby lymph nodes.
Stage I includes cancers that were part of a polyp. If the polyp is removed completely during colonoscopy, with no cancer cells at the edges (margins) of the removed piece, no other treatment may be needed.
If cancer in the polyp is high grade, or there are cancer cells at the edges of the polyp, more surgery might be recommended. You might also be advised to have more surgery if the polyp couldn’t be removed completely or if it had to be removed in many pieces, making it hard to see if cancer cells were at the edges.
For cancers not in a polyp, partial colectomy ─ surgery to remove the section of the colon that has cancer and nearby lymph nodes ─ is the standard treatment. Typically additional treatment may not be needed.
3. Treating stage II colon cancer
Many stage II colon cancers have grown through the wall of the colon, and maybe into nearby tissue, but they have not spread to the lymph nodes.
Surgery to remove the section of the colon containing cancer (partial colectomy) along with nearby lymph nodes may be the only treatment needed. But your doctor may recommend adjuvant chemotherapy (chemotherapy after surgery) if your cancer has a higher risk of coming back (recurring) because of certain factors, such as:
- The cancer looks very abnormal (is high grade) when viewed closely in the lab.
- The cancer has grown into nearby blood or lymph vessels.
- The surgeon did not remove at least 12 lymph nodes.
- Cancer was found in or near the margin (edge) of the removed tissue, meaning that some cancer may have been left behind.
- The cancer had blocked (obstructed) the colon.
- The cancer caused a perforation (hole) in the wall of the colon.
The doctor might also test your tumor for specific gene changes, called MSI or MMR, to help decide if adjuvant chemotherapy would be helpful.
Not all doctors agree on when chemotherapy should be used for stage II colon cancers. It’s important for you to discuss the risks and benefits of chemotherapy with your doctor, including how much it might reduce your risk of recurrence and what the likely side effects will be.
4. Treating stage III colon cancer
Stage III colon cancers have spread to nearby lymph nodes, but they have not yet spread to other parts of the body.
Surgery to remove the section of the colon with cancer (partial colectomy) along with nearby lymph nodes, followed by adjuvant chemotherapy is the standard treatment for this stage.
Chemotherapy regimens are often recommended. With different options and protocols available, you and your doctor will discuss the best treatment plan. The individual’s age and overall health status may be taken into consideration.
For some advanced colon cancers that cannot be removed completely by surgery, neoadjuvant chemotherapy given along with radiation therapy might be recommended to shrink the cancer so it can be removed later with surgery. For some advanced cancers that have been removed by surgery, but were found to be attached to a nearby organ or have positive margins (some of cancer may have been left behind), adjuvant radiation might be recommended. Radiation therapy and/or chemotherapy may be options for people who aren’t healthy enough for surgery.
5. Treating stage IV colon cancer
Stage IV colon cancers have spread from the colon to distant organs and tissues. Colon cancer most often spreads to the liver, but it can also spread to other places like the lungs, brain, peritoneum (the lining of the abdominal cavity), or to distant lymph nodes.
In most cases, surgery is unlikely to cure these cancers. But if there are only a few small areas of cancer spread (metastases) in the liver or lungs and they may be removed along with the colon cancer. Surgery may help the individual live longer. This would mean having surgery to remove the section of the colon containing cancer along with nearby lymph nodes, plus surgery to remove the areas of cancer spread. Chemotherapy is typically given after surgery, as well.
If the metastases cannot be removed because they’re too big or there are too many of them, chemotherapy may be given before surgery (neoadjuvant chemotherapy). Then, if the tumors shrink, surgery may be tried to remove them. Chemotherapy might be given again after surgery as well.
If cancer has spread too much to try to cure it with surgery, chemotherapy is the main treatment. Surgery might still be needed if the cancer is blocking the colon or is likely to do so. Sometimes, such surgery can be avoided by putting a stent (a hollow metal tube) into the colon during a colonoscopy to keep it open. Otherwise, operations such as a colectomy or diverting colostomy (cutting the colon above the level of cancer and attaching the end to an opening in the skin on the belly to allow waste out) may be used.
If the person has stage IV cancer and the doctor recommends surgery, it’s very important to understand the goal of the surgery ─ whether it’s to try to cure cancer or to prevent or relieve symptoms of cancer.
Most people with stage IV cancer will get chemo and/or targeted therapies to control cancer. The choice of regimens depends on several factors, including any previous treatments and the person’s overall health. If one of the regimens is no longer working, another may be tried. For people with certain tumor changes in the MMR genes, another option after initial chemotherapy might be to treat with an immunotherapy drug.
For advanced cancers, radiation therapy may also be recommended to help prevent or relieve symptoms in the colon from cancer such as pain. It might also be used to treat areas of spread such as in the lungs or bone. It may shrink tumors for a time, but it’s not likely to cure cancer. If your doctor recommends radiation therapy, it’s important that you understand the goal of treatment.
6. Treating recurrent colon cancer
Recurrent cancer means that cancer has come back after treatment. The recurrence may be local (near the area of the initial tumor), or it may be in distant organs.
Local recurrence
If cancer comes back locally, surgery (often followed by chemotherapy) can sometimes help you live longer and may even cure you. When cancer can’t be removed surgically, chemotherapy might be tried first. If it shrinks the tumor enough, surgery might be an option. This might be followed by more chemotherapy.
Distant recurrence
If cancer comes back in a distant site, it’s most likely to appear in the liver first. Surgery might be an option for some people. If not, chemotherapy may be tried to shrink the tumor(s), which may then be followed by surgery to remove them. Ablation or embolization techniques might also be an option to treat some liver tumors.
If cancer has spread too much to be treated with surgery, chemotherapy and/or targeted therapies may be used. Possible treatment schedules are the same as for stage IV disease.
For people whose cancers are found to have certain gene changes, another option might be treated with immunotherapy.
Your options depend on which, if any, drugs you had before cancer came back and how long ago you got them, as well as your overall health. You may still need surgery at some point to relieve or prevent blockage of the colon or other local problems. Radiation therapy may be an option to relieve symptoms as well.
Recurrent cancers can often be hard to treat, so you might also want to ask your doctor if clinical trials of newer treatments are available. (5)
Summary
Colon cancer is a very real threat to those of us in the Baby Boomer generation. Hereditary factors and lifestyle are the main risk factors in play. This Blog page is intended to provide some basic knowledge about Risks, Screening, Prevention, and Treatments. This does not take the place of information or recommendation made by the individual’s physician. If you have learned anything from this page, you will truly understand the importance of both lifestyle changes and screening.
So, if you have not been screened for colorectal cancer recently, it is time to check with your physician and GET SCREENED.
References:
- https://www.cdc.gov/cancer/colorectal
- https://bloomerboomer.com/get-screened-for-colon-cancer/
- https://www.cancer.org/health-care-professionals/american-cancer-society-prevention-early-detection-guidelines/colorectal-cancer-screening-guidelines.html
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/colon-cancer/colon-cancer-symptoms
- https://www.cancer.org/cancer/colon-rectal-cancer/treating/by-stage-colon.html